The awareness campaigns for depression are bothersome. Which may seem like a cold-hearted comment for anyone dealing with it, or anyone that has a friend or family member dealing with it, but not when you take a look at what’s causing it.
Perhaps frustrating would have been a better word than bothersome, as the main problem with the message is that they’re telling us it’s unavoidable. Implying that depression is on the rise for some unexplainable reason, and we better cross our fingers and hope we don’t get it, or try to cope with it via psychiatric appointments and anti-depressants (the most common prescription in the U.S. by the way).

Realistically, there’s PLENTY you can do about it…if you’re willing to try. But I’ll warn you up-front that it extends well beyond talking about it, and popping the latest wonder drug. Regardless of how much Big Pharma and Sam the Shrink tells you it’s a chemical imbalance problem!
More specifically, it involves keeping an open mind. Since getting to the root of the problem requires accepting that your diet may be causing it, which is often thought of as “placing blame.”
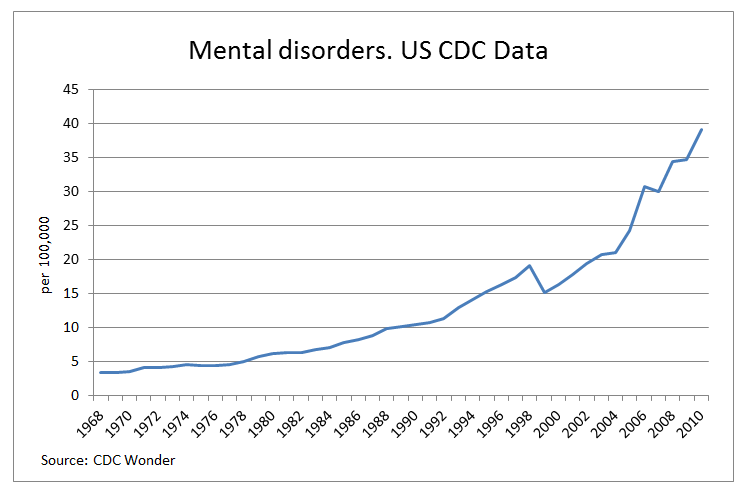
But, as you’ll discover, NONE of this is your fault. Because if it was, we wouldn’t see it affecting an enormous chunk of the population (along with a variety of other mental conditions), and we wouldn’t haven’t seen a steady increase that’s paralleled a reduction in saturated fat, an explosion in carbohydrates and polyunsaturated oils, and an ever-climbing rise in obesity and diabetes.
In short, the dietary advice of the last 50 years has created an environment where our brain is flooded with glucose and inflammation, and starved of essentials and protection. Or to put it bluntly:
The Standard American Diet is making Depression the American Standard.
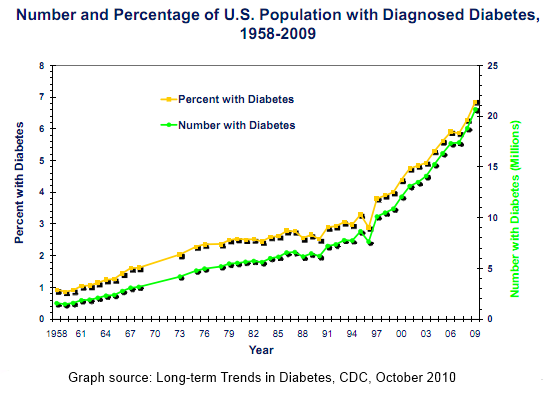
For instance, the latest government statistics suggest that we’ve reduced our intake of saturated fat by approximately 11% compared to 40-45 years ago, and replaced those brain boosting, cell-supporting essentials with a 25% increase in (non-essential) carbohydrates. Not only producing the highest levels of obesity and diabetes in history, and increasing a long-list of mental and physical conditions associated with hyperglycemia and insulin resistance, but putting us in a chronic state of inflammation and creating deficiencies that have serious implications for our cognitive health and performance.
“Insulin resistance and severity of depressive symptoms were positively correlated, particularly in people with impaired glucose tolerance.” BMJ, 2005

The lack of fat in the diet is an obvious place to start, because without it we fail to absorb many of the “brain-selective” nutrients that gave us our sizeable brain in the first place. And likewise, we fail to acquire many of these nutrients in the diet, because the fat-rich animal protein sources where they’re located are commonly avoided – including the saturated fat and cholesterol itself.
Of these essentials, the omega-3 essential fatty acids are probably the most significant. Since our brain needs a regular dose of DHA, and this long-chain form (not to be confused with the plant-based, short-chain ALA) is only properly obtained from animal source foods (1, 2). Meaning, those restricting meat and fish, and specifically the fat from meat and fish, are missing out.
Sadly, we’ve also seen a considerable increase in omega-6 fatty acids, which compete with omega-3’s and kick us into a pro-inflammatory state. Partly because people are wrongfully encouraged to follow plant-based diets, but mainly because the use of vegetable and seed oils (PUFAs) has skyrocketed:
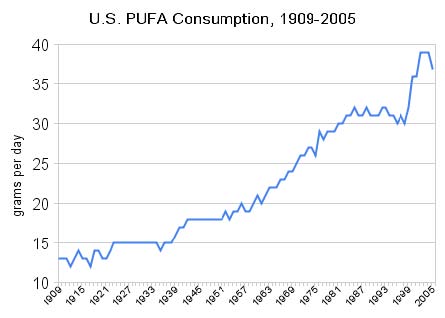
Consequently, this moves us from the ideal omega 6:3 ratio of 1:1, to a 25:1 ratio and a chronic state of inflammation – which along with an omega-3 deficient brain, leads to a damaged one, and an increased risk of anxiety, depression (1, 2, 3, 4, 5, 6, 7) and other mental conditions. Largely because of the inflammation, but also because of the oxidation (1, 2); since these vegetable and seed oils morph into free radicals when they’re exposed to heat, light, or oxygen.
Good thing we’re only cooking with them! (insert sarcasm)
The next obvious deficiency is B12. That despite getting no media attention, and rarely getting tested for, affects more than 40% of the population between the ages of 26 and 83. With that number jumping up significantly when you recognize that the standards for plasma levels in the U.S. (200-350pg/mL) are far too low, and the fact that normal levels don’t necessarily mean adequate B12 (also known as a ‘functional deficiency’)

One of the reasons for this epidemic is because the type of B12 humans need (cobalamin) is only obtainable from animal products; while the plant-based pseudo B12 (cobamide) actually increases our need. Hence the reason vegetarians are vegans are more deficient than the general population (1, 2); especially when using the more advanced testing for B12, instead of the traditional (unreliable) blood tests.
Research suggests that 68% of vegetarians and 83% of vegans are B12 deficient.
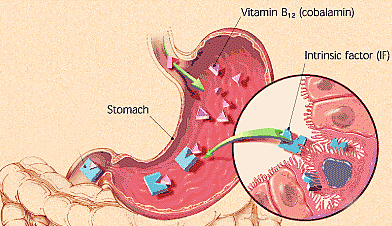
The other reason deficiency is common is because of poor digestion. People are walking around with damaged guts that aren’t producing adequate stomach acid to breakdown their food, and thus aren’t absorbing the nutrients. So even when they do eat meat and fish, they’re not absorbing B12, and they’re becoming (or remaining) deficient.
This is a point that’s highlighted when you understand that B12 specifically requires the intrinsic factor, and this tends to down-regulate for those that not actively stimulating it with meat.
The reason B12 is so important for the brain and nervous system, is because it helps produce the protective outer layer (myelin sheath) that surrounds our nerves. Meaning, those who aren’t getting enough B12, are not not getting that protection, and are therefore increasing their risk of the various cognitive and neurological conditions associated with nerve damage (just like vegetarians do).
According to a study from 2008 in the journal Neurology, those with the highest levels of B12 were 6 times less likely to have brain shrinkage than those with the lowest.
Cholesterol has a similar role in the brain, as it helps build cell membranes and feed and support the neurons and their various functions (myelin included). It also helps maintain adequate nutrient levels (vitamin D specifically), and protect against oxidation. Which is arguably why we see our cholesterol levels naturally increase with age, and it’s DEFINITELY why we don’t want to restrict our saturated fat intake (that raises it) or try to lower it with pharmaceuticals.

What the statin salesman won’t tell you is that low cholesterol levels are associated with depression, aggression, cognitive impairment, degenerative brain conditions (Alzheimer’s), and neurological disorders (Parkinson’s); while the statins themselves appear to prevent the beneficial effects of omega-3 supplementation (along with MANY other adverse health effects).
Though what’s worse, is that individuals classified as ‘high-risk’ because of ‘high-cholesterol’ are the same ones advised to drop the butter and embrace the canola, sunflower, and soybean because they ‘lower cholesterol.’ Not only moving them away from an anti-inflammatory food to a pro-inflammatory one and skewing the omega 6:3 ratio towards a chronic state of inflammation, but exposing these people to the other driver of nerve and arterial damage – OXIDATION!
Throw in the “heart healthy,” “high-fiber,” whole grains, and it’s pretty easy to see how:
The unnecessary fears of fat (from 1970 to today) have robbed our brain of the essentials, and supplied it with a consistent dose of damage.
This is true whether we’re looking at the hyperglycemia (chronically elevated blood sugar) and chronic inflammation from an over-reliance on gut-damaging insulin-spiking replacements, the nutrient deficiencies and heightened susceptibility to brain damage because of a lack of fat and cholesterol-rich animal products (we’ve always consumed), or the consistent rise of obesity, diabetes, and heart disease that eventually occurs as a result – and elevates our risk of cognitive impairment.
Cognitive impairment (decline in brain performance) increases by 220 percent if you develop diabetes before age 65. Diabetics are twice as likely to develop Alzheimer’s disease and 1.75 times more likely to develop dementia of any kind.
Conventional wisdom is going to tell you otherwise, and suggest that I’m a heartless, insensitive bastard (or quack), but any rationale person would have trouble ignoring the evidence. Especially when they recognize that this excess inflammation and lack of protection is also damaging the gut (which has a direct impact on the health and performance of our brain), and the over-use of antibiotics and other gut-permeating, brain-damaging behaviors (sleep, sunshine, stress) have accompanied this crappy diet.
But whatever the case, the one thing we do know, is that you can’t get better unless you try. So why not give it a shot?
Stay Lean!
Coach Mike
RELATED ARTICLES:
More Antibiotic = Less Probiotic
The Best Thing You Can Do For Your Brain
High Blood Sugar (Hyperglycemia) AGEs The Body
Don't Mess With the Microbes - Gut Bacteria, Obesity & Disease
Asthma, Eczema, Headaches, IBS, Arthritis, Depression? Go WIth Your Gut