The hottest trend in 21st century research (at the time of writing this post) is swapping the gut microbes of mice to pinpoint the impact of different bacterial strains on our health and body composition. With various studies showing considerable evidence that a bacteria-shift alone can turn a lean mouse into a fat mouse (1, 2), a normal eater into an overeater (1, 2, 3), and a glucose-tolerator into an insulin-resister (in only 14 days!)
Yes, the studies are done on mice – which have a very different bacterial makeup in their gastrointestinal system than humans – but the two dominant strains (Bacteriodetes & Firmicutes) are the same, and the microbial alterations appear to affect humans just as much. With the composition of our gut bacteria having a direct impact on energy metabolism, insulin sensitivity, immune function (1, 2), body-fatness, and long-term health (1, 2, 3).
But more importantly, what we eat and what we expose ourselves to (1, 2, 3, 4, 5), has a direct influence on this microbial makeup.
Gone are the days of believing that our gut microbiota remains stable once it’s established as an infant (1, 2, 3, 4, 5, 6). As recent findings clearly show dramatic changes after drug treatment, and considerable differences from dietary input. Meaning, our day-to-day behaviour can cause long-term alterations to our gut microbiota that positively or negatively affect our health and body composition. Whether we’re a growing-child (1, 2) or a fully-developed adult (1, 2, 3)!
Frankly, this shouldn’t come as a surprise. Given that we have 10 times more bacteria in our intestine than cells on our entire body; and given that the microbiota is essentially a tenant in our gut, with 100-150 times more genes than the human genome (1, 2).
If we were smart, we’d be doing our best to keep this creature (our neighbour) happy. Considering it has the ability to turn our genes on or off (Bacteriodetes can alter over 400 of them) based on what we feed it, and how we treat it. And considering the healthier it is, the healthier we are, whether we’re talking about immune protection and disease prevention, obesity and insulin resistance, or physical and cognitive performance (1, 2, 3, 4, 5).
But sadly, most of us haven’t been taking care of our microbiota; especially over the last 50 years. As we’ve disrupted it’s home, cut off it’s food supply, and attacked it directly with antibiotics, crappy foods, and chronic stress. Leaving behind a gastrointestinal environment overthrown by unfriendly bacteria (dysbiosis), chronically exposed to inflammation, and ready to break – if it hasn’t already.
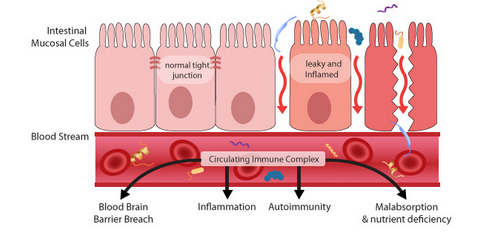
A permeable gut is linked to degenerative conditions that extend well beyond gastrointestinal inflammation (like Chron’s and Colitis) – with this study linking more than 100 diseases! And the latest research suggesting that the significant rise in auto-immune conditions, is because of disrupted microbes that would have otherwise protected against invading pathogens and unnecessary intestinal distress.
Arguably, this is the result of rampant antibiotic use over the last 50 years (1, 2, 3, 4, 5, 6). Since one of these treatments alone can wipe out beneficial gut bugs for years to come. With this study showing no signs of the missing bacteria for over 2 years…and that was a SINGLE 7 day course of antibiotics!
Although, there are a long list of other contributing factors that have also increased over this time period. That all result in the same outcome – a weakened defense system overburdened by harmful bacteria.
- Method and delivery of birth – c-section discouraged (1, 2, 3, 4)
- Parents gut health and mothers diet during pregnancy
- Infant’s transition from breast milk to adult food
- Current diet (1, 2, 3, 4, 5, 6)
- Environmental exposure – pesticides, PCBs, herbicides, arsenic, BPA, etc
- Disease status – current health and body comp (1, 2, 3)
- Other chronic medication use – NSAIDs, anti-depressants, antacids, etc
Call it the perfect storm if you will; or maybe the breaking point. As we’ve somehow managed to wipe out good bacteria, add in bad bacteria, make sure it stays fed, and prevent it from getting fixed. Leading to a leaky gut for some, bacterial overgrowth for others, and a long-list of unexplained (and supposedly untreatable) gastrointestinal, psychological, emotional, neurological and dermatological symptoms for everybody else.
(Not to mention that whole obesity problem).
If you’re not experiencing any health issues, you’re one of the lucky ones. As depression, autism, asthma, diabetes (type 1 and 2), arthritis (1, 2), fibromyalgia, Parkinson’s, Narcolepsy, inflammatory bowel disorders (IBS, Chron’s, Colitis), inflammatory skin conditions (psoriasis, eczema), hypothyroidism, chronic fatigue syndrome, Schizophrenia, Multiple sclerosis, lupus, kidney disease, and infertility continue to be on the rise; and disrupted gut health provides a reasonable explanation as to why. Especially when we’re talking about degenerative conditions related to the the brain and central nervous (1, 2, 3, 4, 5, 6)
Not every disease is the result of a leaky gut, and not everyone will develop a leaky gut, but with the evidence we have to-date (over 10,000+ papers) this 100-year old hypothesis is no longer quackery (1, 2). And everyone (regardless of good genes) should be taking the necessary dietary and lifestyle steps to improve the integrity of their gut lining, and support their bacterial buddy. Since the degenerative consequences of a messed-up microbiota are devastating enough on their own – obesity, diabetes, heart disease, Alzheimer’s, etc.
- Try a Grain and Sugar-Free Intervention – to starve unfriendly bacteria
- Stop using bacteria-destroying medications (NSAID’s, antibiotics, pharmaceuticals) – to prevent future damage
- Add more Coconut Oil and Vinegar to your regimen – to disinfect GI tract
- Test your Digestion and consider an HCL supplement – to ensure stomach acid is adequate
- Introduce Fermented Foods or a Probiotic supplement – to repopulate beneficial bacteria
- Keep taking Zinc and Fish Oil – to strengthen the gut lining (1, 2) and reduce inflammation
- Consider a Yeast/Parasite killing supplement – to get rid of candida, h. pylori, etc
The 7th recommendation isn’t a requirement, but given that more than 50% of the population has unknowingly been affected with h. pylori, and given that this could be driving low stomach acid and disrupted gut health, it’s worth considering. You’ll also want to work on actively reducing stress. Since just like the gut can negatively affect the brain, our brain can negatively affect our gut – shutting down the gastrointestinal system (poor digestion and elimination) and promoting inflammation in times of stress, and making us more susceptible to infection, overgrowth, and permeability (1, 2, 3, 4, 5, 6, 7).
This starts with prioritizing sleep, and finishes with reducing sympathetic stressors and/or making time for parasympathetic activities – like low-intensity activity, meditation, enjoyable hobbies, and play.
“The control of man’s diet is readily accomplished, but mastery over his intestinal bacterial flora is not.” –Bond Stow, 1914
Again, not everyone has holes in their gut, or the auto-immune conditions that develop as a result, but everyone has the potential to develop them; and probably has the unfavorable ratio of good-to-bad bacteria that precedes it. Especially if they’re eating anywhere close to a diet that resembles the Standard American Diet, they’ve done a round or 2 of antibiotics, and they’ve been exposed to a considerable dose of environmental toxins, pharmaceutical drugs, and stress.
Which seems to be juuussst about everyone…
Stay Lean!
Coach Mike
RELATED ARTICLES:
More Antibiotic = Less Probiotic
Zonulin - Connecting Wheat & Leaky Gut
Beyond Live It NOT Diet! - Test Your Digestion
