Resistant starch is the latest craze in nutrition. And like most things that ‘all of a sudden burst onto the scene out of nowhere,’ we’re being told that it can solve all of our health problems with little to no other change in our diet and lifestyle.
But this time it’s not just Dr. Oz and the celebrity trainers promising 10 pounds in 10 days, it’s Paleo folks, low-carb advocates, and a lot of highly-respected health professionals recommending it. Largely because resistant starch is unique in it’s ability to lower the blood glucose response from the meal we’re eating (like traditional fiber), while acting as a fuel source for the beneficial bacteria in our gut (like the prebiotics in fruits and vegetables).
Or at least that’s how it’s supposed to work.
As we’ve discussed in the past, an isolated component from a specific food is a lot different than the real food itself, so supplementing it may not be a wise decision. Likewise, consuming a food strictly because it has something in it may not be either, as we need to see if the potential upside outweighs the downside.
Similar to fiber, resistant starch itself does not spike blood glucose or count as calories, because it skips digestion and basically registers as ‘nothing’ until it reaches the colon. But, this doesn’t mean the compounds that accompany it have the same impact. And unfortunately for resistant starch, it’s commonly attached to high-glycemic starchy carbohydrates (rice, beans, potatoes, etc). Leaving us with a simple question of whether or not the blood sugar spike and carbohydrate load is worth it?
For ‘most people’ reading this, it’s not. Because, ‘most people’ are obese, insulin resistant, and sedentary. Meaning, all the resistant starch in the world isn’t going to improve their situation…and may in fact make it worse! Especially if we’re talking about replacing animal protein or low-glycemic vegetables with more rice and beans.

Moreover, when reviewing the resistant starch evidence, it’s clear that the positive improvements in insulin sensitivity, glycemic response, and cardiovascular biomarkers are seen when comparing it to rapidly digesting carbohydrates (1, 2, 3).
For instance, in this specific study from 2006 in the journal Diabetes Care, the researchers compared straight glucose (at 1g/keg of bodyweight) to muffins with soluble fiber and resistant starch. And of course the resistant starch produced lower blood and insulin levels (than straight sugar)!
Or this study from Tokyo in 2004, comparing resistant corn starch to corn starch.
How about corn nothing?
Similar to the positive research on fiber, we’re obviously going to see benefits in the short term when adding resistant starch to someone’s crappy diet that doesn’t consume it now – because it will fill them up, make sure they don’t absorb their McDonalds, and improve their health for a few weeks. But compare it so someone eating steak and a salad, or a piece of fish and some broccoli, and the blood sugar and insulin response is going to be worse. And more than likely, the long-term impact will be negative.
…just like it is with fiber:
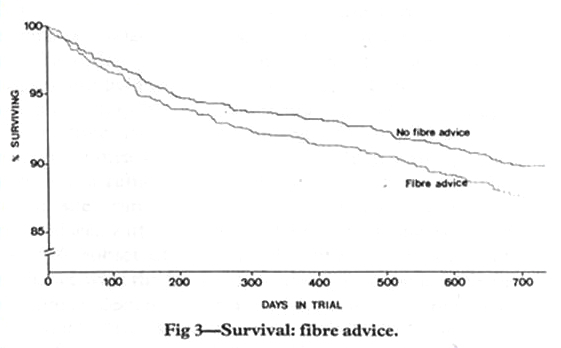
The reality is, most of the promising research on resistant starch and gut health appears to be misleading (1, 2), with most of the studies comparing it to corn starch and traditional fiber – and not really proving anything at all. Conversely, if we compare these resistant starches to a boatload of fermentable fruits and vegetables the result would be quite different (especially if we cook em’ in butyrate-rich butter!)
Or simply put, just like fiber isn’t a good enough reason to eat grains, it seems resistant starch isn’t a good enough reason to prioritize high-carb plants. As yes, rice and beans are high in resistant starch, but meat and greens are still a better choice. And there’s plenty of soluble fibers and prebiotics (inulin, FOS) you can consume elsewhere (even in nuts and seeds) that will produce butyrate.

Sadly, resistant starch seems to be going the way of fiber, with people across the globe turning to supplementation (raw potato starch) to avoid the glucose-load and insulin elevations that come with rice, legumes, and plantains (all high in resistant starch). Which not only seems like a bad idea because of what we know about insoluble fiber and nutrient absorption, but because:
We don’t know whether straight resistant starch affects the gut the same way as the diverse combination of fibers found in whole food!
But most importantly, the majority of the population is already walking around with a damaged gut – from antibiotics, toxins, minimal microbes, etc. Meaning, a large bolus of bacteria-feed to a gastrointestinal system with dysbiosis and dealing with fungus and pathogenic microbiota.
Oops!

Not to bombard you with information, but the latest evidence is showing that at least 25% of the population (probably more when you consider the unhealthy) doesn’t have the bacterial species (Ruminococcus bromii) necessary to break down RS2 and RS3. And that high-dose RS2 supplementation (i.e. raw potato or banana starch) appears to reduce critical health-boosting bacterial strains, like Bifidobacteria longum and Akkermansia muciniphila (1, 2). The same ones that are already depleted via Standard-American living, and the same ones that are boosted via the prebiotics found in fruits and vegetables.
Or put another way, you shouldn’t supplement raw potato starch, just like you shouldn’t supplement inulin or fiber. The majority of the population should be focusing on starving and killing bad bacteria, or repopulating with beneficial strains, not over-feeding what’s already there.

Likewise, you shouldn’t be prioritizing resistant starch foods; especially if you’re obese, insulin resistant, sedentary, or working with a damaged gut (which you probably are). Bad bacteria eats sugar, so telling someone to consume more of it doesn’t help their gut health or their body composition; no matter how you decide to spin it.
Realistically, you can get all the good bacteria support you need by prioritizing vegetables daily and consuming fruits and starchy tubers where appropriate. This will give your gut the soluble fiber it needs to create anti-inflammatory short-chain fatty acids (like butyrate) via fermentation, and ensure you have a healthy balance. In contrast to the potential overgrowth of bad bacteria that could occur from prioritizing high-carb foods for the sake of resistant starch.
Stay Lean!
Coach Mike
RELATED ARTICLES:
Test Your Digestion (The HCL Test)
Beyond Live It NOT Diet! - Repair Your Gut
10 Benefits of Low-Carb You Don't Get With Other Diets
FODMAPs - Fancy Word For Fart-Stopper? That's Worse For Your Gut?